Antiplatelets
If you haven't had a look at the physiology of platelets yet, have a quick look at the notes on their normal function before we have a trek through the different drugs that affect them (just click here).
Aspirin
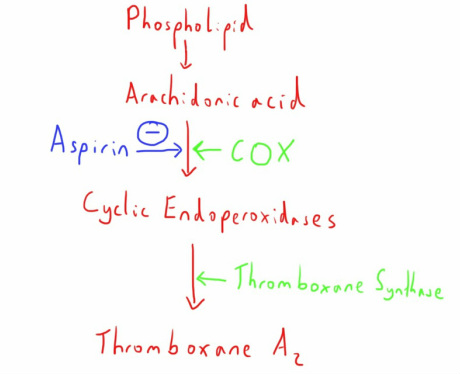
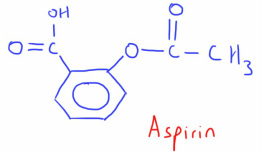
Aspirin (Acetylsalicylic Acid) acts by inhibition of the platelet cyclo-oxygenase type 1 (COX-1) enzyme system.
This is the enzyme system that produces Thromboxane-A2 de novo in activated platelets which has strong pro-coagulant effects.
It also has it's analgesic effects through this COX-1 inhibition, similar to other NSAIDs.
As the platelet has no nucleus it is unable to resynthesise these inactivated enzymes and so the therapeutic action will exist for the lifespan of the platelet.
This is the enzyme system that produces Thromboxane-A2 de novo in activated platelets which has strong pro-coagulant effects.
It also has it's analgesic effects through this COX-1 inhibition, similar to other NSAIDs.
As the platelet has no nucleus it is unable to resynthesise these inactivated enzymes and so the therapeutic action will exist for the lifespan of the platelet.
Pharmacokinetics
Aspirin is a weak acid with a pKa of 3.
As a result it exists in an almost entirely unionised form in the stomach after ingestion, in theory allowing more rapid uptake.
However the relative alkaline conditions of the mucosa cause some sequestration of the molecule here, and the majority of uptake is via the larger surface area of the small intestine.
As a result it exists in an almost entirely unionised form in the stomach after ingestion, in theory allowing more rapid uptake.
However the relative alkaline conditions of the mucosa cause some sequestration of the molecule here, and the majority of uptake is via the larger surface area of the small intestine.
It is fairly highly protein bound in the plasma (85%).
It undergoes metabolism by esterases in both the liver and the intestine, with its metabolites (e.g. salicylate) being excreted in the urine.
It undergoes metabolism by esterases in both the liver and the intestine, with its metabolites (e.g. salicylate) being excreted in the urine.
A loading dose of 300mg will take only about 30 mins to have a maximal effect.
Adverse Effects
These are similar to other NSAIDs as they arise from the effects of COX inhibition.
These side effects are less notable when the therapeutic dose of 75mg is used, with the effects being primarily limited to the platelets.
These side effects are less notable when the therapeutic dose of 75mg is used, with the effects being primarily limited to the platelets.
- Gastric irritation - Of varying severity. Prostaglandins than are produced by the same COX pathway have an important regulation/protective role in the stomach mucosa. The sequestration of aspirin in this area may potentiate these side effects.
- Renal dysfunction - In a similar way, prostaglandins also play an important role in renal blood regulation and disruption of their synthesis can lead to renal dysfunction.
- Asthma - Certain asthmatics may be sensitive to NSAIDs and experience a deterioration in their asthma. This may be due to the increased amount of arachidonic acid that is converted to exacerbating leukotrienes when the COX pathway is inhibited.
- Reyes Syndrome - a severe multisystem condition that can rarely follow use of aspirin in children or adolescents with a viral illness.
Clopidogrel
Clopidogrel acts by binding to the purinergic P2 receptors on the surface of platelets.
These receptors are where ADP binds and acts to activate platelets.
In particular, clopidogrel prevents the upregulation of the IIb/IIIa glycoproteins that are a core part of platelet aggregation.
As with aspirin this binding is irreversible and the platelet is unable to synthesize further receptors.
These receptors are where ADP binds and acts to activate platelets.
In particular, clopidogrel prevents the upregulation of the IIb/IIIa glycoproteins that are a core part of platelet aggregation.
As with aspirin this binding is irreversible and the platelet is unable to synthesize further receptors.
Pharmacokinetics
Clopidogrel is a prodrug which is activated in the liver.
It has good intestinal absorption but the onset of action is slow and it usually given as a loading dose of 300mg compared with the maintenance dose of 75mg.
The active metabolite has a half life of approximately 8 hours before hepatic metabolism.
It has good intestinal absorption but the onset of action is slow and it usually given as a loading dose of 300mg compared with the maintenance dose of 75mg.
The active metabolite has a half life of approximately 8 hours before hepatic metabolism.
Adverse Effects
- Abdominal upset - Relatively common with dyspepsia, diarrhoea and pain
- Bleeding - As with the other anticoagulants, an obvious increased risk of bleeding
Dipyridamole
Dipyidamole is a phosphodiestarase inhibitor.
This has several important effects on platelet function:
These actions result in reduced levels of upregulation of the GPIIb/IIIa receptors and impairs platelet adhesion.
It also potentiates the activity of prostacyclin and so has vasodilating properties.
This has several important effects on platelet function:
- Increases levels of cAMP, reducing intracellular calcium ion levels
- Inhibits uptake of adenosine it to the platelets
These actions result in reduced levels of upregulation of the GPIIb/IIIa receptors and impairs platelet adhesion.
It also potentiates the activity of prostacyclin and so has vasodilating properties.
Adverse Effects
- Flushing and hypotension - resulting from vasodilation
- Headache - Also from its vasodilating properties
- Gastrointestinal upset
GP IIb/IIIa Receptor Antagonists
A group of medications reserved for use on a short term basis around acute coronary events.
They act by blocking the GPIIb/IIIa receptors which are required for platelet aggregation, thereby having a powerful effect on platelet function.
They do not, however, interfere with the other functional roles that platelets are part of e.g. release of pro-coagulant factors.
They act by blocking the GPIIb/IIIa receptors which are required for platelet aggregation, thereby having a powerful effect on platelet function.
They do not, however, interfere with the other functional roles that platelets are part of e.g. release of pro-coagulant factors.