Platelets
As a vital component of the body's haemostatic mechanisms and as a target for a number of different drugs, a decent understanding of platelet physiology is useful for all medical specialties.
Production
Platelets (thrombocytes) can be considered as fragments of larger precursor cells called megakaryocytes.
These cells exist in the bone marrow as a lineage of the pluripotent stem cells.
Megakaryocytes, under the influence of thrombopoietin, undergo maturation in the bone marrow.
During this time (about 10 days from stem cell to platelet), the megakaryocyte undergoes a period of significant growth.
There is significant DNA replication and enlargement of cytoplasmic volume but without cell division, ultimately producing a cell with multiple nuclei and a highly granulated cytoplasm.
When this mature megakaryocyte stage is reached the cell starts to fragment, resulting in between 1000 and 5000 platelets.
These cells exist in the bone marrow as a lineage of the pluripotent stem cells.
Megakaryocytes, under the influence of thrombopoietin, undergo maturation in the bone marrow.
During this time (about 10 days from stem cell to platelet), the megakaryocyte undergoes a period of significant growth.
There is significant DNA replication and enlargement of cytoplasmic volume but without cell division, ultimately producing a cell with multiple nuclei and a highly granulated cytoplasm.
When this mature megakaryocyte stage is reached the cell starts to fragment, resulting in between 1000 and 5000 platelets.
Thrombopoietin is constantly synthesised by the liver and kidneys.
It acts on megakaryocyte receptors to stimulate the quantity and rate of megakaryocyte maturation.
It's regulating mechanism is interesting as it is achieved by binding of the thrombopoietin to receptors on the platelets themselves: the more platelets circulating, the more binding of thrombopoietin and the less circulating in the blood.
It acts on megakaryocyte receptors to stimulate the quantity and rate of megakaryocyte maturation.
It's regulating mechanism is interesting as it is achieved by binding of the thrombopoietin to receptors on the platelets themselves: the more platelets circulating, the more binding of thrombopoietin and the less circulating in the blood.
Platelets normally have a lifespan in the circulation of 7-10 days, though this can be significantly reduced is conditions such as splenomegaly.
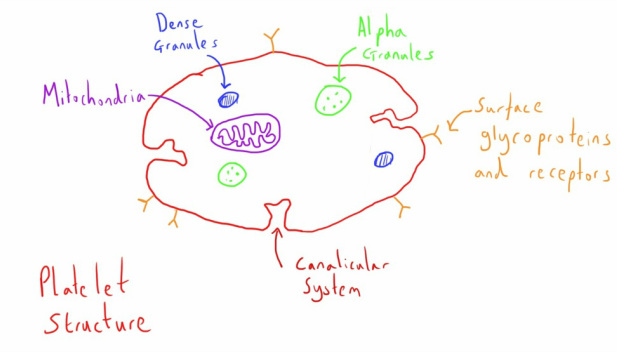
Structure
Platelets are small disc like structures about 3 micrometers in diameter.
Their most striking feature is that, as they are fragment of the megakaryocytes, they do not possess their own nuclei.
As a result they are unable to synthesise their own proteins.
Their most striking feature is that, as they are fragment of the megakaryocytes, they do not possess their own nuclei.
As a result they are unable to synthesise their own proteins.
Whilst many of the important structures can be seen in the diagram above, most are best discussed in the context of their function (below).
The cannalicular system of the platelet acts to provide a large surface area of platelet phospholipids for several reactions in the coagulation pathway which requires these phospholipids.
The cannalicular system of the platelet acts to provide a large surface area of platelet phospholipids for several reactions in the coagulation pathway which requires these phospholipids.
Function
Platelets play a central role in haemostasis and it is difficult to talk about their function without considering the other components of haemostasis (talked about here).
However, I have found is easier to understand the overall picture of haemostasis if some of the specific structural and metabolic features of platelets are discussed.
However, I have found is easier to understand the overall picture of haemostasis if some of the specific structural and metabolic features of platelets are discussed.
As a short synopsis, platelets undergo 3 roles in haemostasis:
- Adhesion - Adhering to the subendothelial substances after vessel wall injury and acting as an important starting point for the entire haemostasis process.
- Activation - Triggered by adhesion and by simultaneous factors in the coagulation cascade and neighbouring platelets, platelets become activated and change their structure and release a large number of factors to promote the process of haemostasis. This role is absolutely central to successful haemostasis due to it's impact on the coagulation cascade and the positive feedback on other platelets.
- Aggregation - After activation platelets begin to aggregate to each other, forming the initial platelet plug and continuing to be the basis for the final fibrin clot
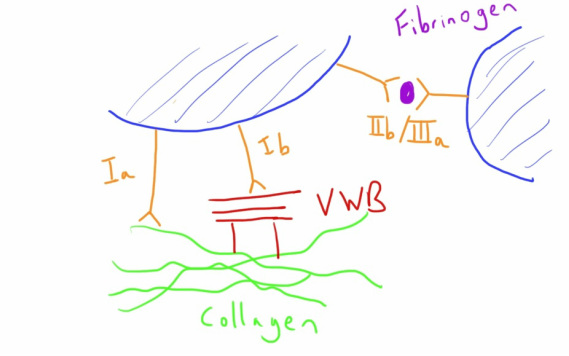
Glycoproteins
The platelets glycoproteins play a core role in all of the platelet's aforementioned actions so seem a good place to start. There are 3 of interest to us:
- GP Ia - This glycoprotein is involved in the initial adhesion to subendothelial collagen, adhering the platelet to the subendothelial tissue and in the process activating the platelet.
- GP Ib - Is very similar to GPIa but adheres via the medium of the protein Von Willebrand Factor (VWF). It also activates the platelet in the process of adhesion.
- GPIIb/IIIa - On an 'unactivated' platelets these glycoproteins have little function. They undergo a large degree of up-regulation after a platelet has been activated and contribute to increased adhesion to VWF in the same manner as GPIb. The important difference is that these are able to adhere to fibrinogen molecules and through these bridges aggregate with other activated platelets.
So the role of the different glycoproteins in adhesion and aggregation is hopefully fairly clear, as well as how they play a role in platelet activation.
Activation
Activation of platelets plays a central role in the whole haemostasis process.
Activated platelets:
Activated platelets:
- Can aggregate to form a platelet plug
- Provide a platform for the coagulation cascade
- Provide factors for the coagulation cascade
- Provide positive feedback to activate other platelets
Platelets can be activated by:
- Adhesion through GPIa or GPIb glycoproteins
- Soluble activators (ADP, Thromboxane A2, Thrombin, Serotonin)
When activated, platelets undergo several changes:
- Structural reconfiguration with increased exposure of the platelets phospholipids that act as a platform for parts of the coagulation cascade
- Release of stored alpha granules and dense granules
- Activation of GPIIb/IIIa receptors
- Thromboxane A2 synthesis
Alpha granules contain:
- Fibrinogen - A substrate for the coagulation reactions
- Von Willebrand Factor - A carrier for factor VIII and important for platelet adhesion
- Certain cytokines
Dense granules contain:
- ADP - A potent activator of other platelets that is one of the key positive feedback loops
- ATP - An energy source
- Serotonin - A potent vasoconstrictor
- Adrenaline - Another potent vasoconstrictor
Adenosine diphosphate (ADP) is one of the key substances released during platelet activation.
It acts in a positive feedback role to promote activation of surrounding platelets.
In addition, it triggers the platelet to upregulate it's GP IIb/IIIa receptors to allow platelet aggregation.
It acts at purinergic P2 receptors on platelets, which happen to be the target of the antiplatelet drug clopidogrel.
It acts in a positive feedback role to promote activation of surrounding platelets.
In addition, it triggers the platelet to upregulate it's GP IIb/IIIa receptors to allow platelet aggregation.
It acts at purinergic P2 receptors on platelets, which happen to be the target of the antiplatelet drug clopidogrel.
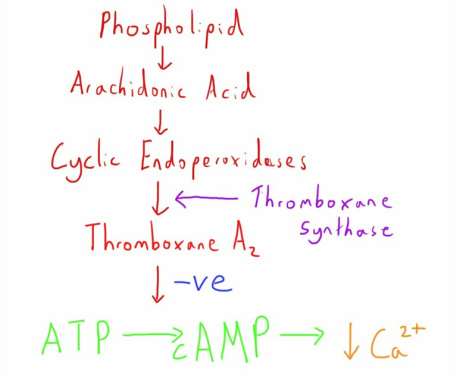
Thromboxane A2 is another important substance which is synthesised afresh when platelets are activated and which also goes on to positively feedback and active other platelets.
In addition to activating surrounding platelets it acts as a potent vasoconstrictor, further helping with haemostasis.
It's synthesis is disrupted by aspirin and is the mechanism of action for the drug's antiplatelet activity.
It is naturally unstable and broken down quickly, limiting it's effect site to the area of release.
In addition to activating surrounding platelets it acts as a potent vasoconstrictor, further helping with haemostasis.
It's synthesis is disrupted by aspirin and is the mechanism of action for the drug's antiplatelet activity.
It is naturally unstable and broken down quickly, limiting it's effect site to the area of release.
Thromboxane A2 has its effect by suppressing the levels of platelet cyclic adenosine monophosphate (cAMP).
cAMP acts to regulate the levels of calcium, with high cAMP resulting in low calcium ion levels.
Calcium is an important part of activation and aggregation, so the inhibition of cAMP formation by thromboxane A2 allows increased calcium ions to achieve this.
cAMP acts to regulate the levels of calcium, with high cAMP resulting in low calcium ion levels.
Calcium is an important part of activation and aggregation, so the inhibition of cAMP formation by thromboxane A2 allows increased calcium ions to achieve this.
Prostacyclin is an alternative product of the cyclic endoperoxidase pathway (prostacyclin synthase as the enzyme instead).
This is synthesised by normal endothelium and has the opposite effects to thromboxane A2 and increases platelet levels of cAMP.
Through this mechanism you can see how the normal endothelium can have an anti-platelet effect.
This is synthesised by normal endothelium and has the opposite effects to thromboxane A2 and increases platelet levels of cAMP.
Through this mechanism you can see how the normal endothelium can have an anti-platelet effect.
Antigens
Platelets have ABO antigens in the same way that red cells do, and hence this needs testing for appropriately prior to transfusion.
They also possess human leucocyte antigen (HLA) class 1 antigens and antigens specific to platelets named human platelet antigen (HPA).
In patients who undergo multiple platelet transfusions there is the potential for development of antibodies to these antigens
They also possess human leucocyte antigen (HLA) class 1 antigens and antigens specific to platelets named human platelet antigen (HPA).
In patients who undergo multiple platelet transfusions there is the potential for development of antibodies to these antigens