Heparin
To understand how heparin acts we need to cast our mind back to the natural anticoagulant mechanisms of the whole haemostasis equilibrium (some more on this here).
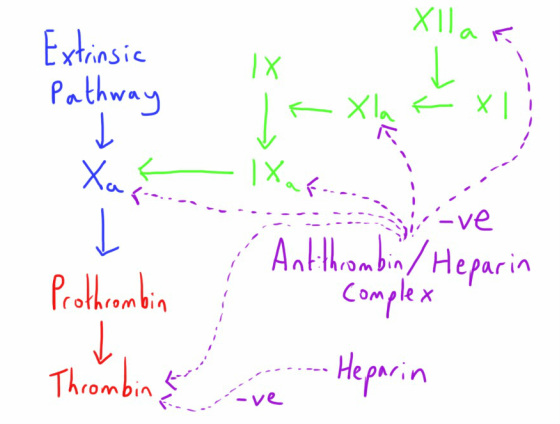
The endogenous molecule Antithrombin III acts as an anticoagulant by binding to and inhibiting several of the pro-coagulant clotting factors; most notably thrombin and factor Xa (but also factors IXa, XIa and XIIa).
The endogenous molecule Antithrombin III acts as an anticoagulant by binding to and inhibiting several of the pro-coagulant clotting factors; most notably thrombin and factor Xa (but also factors IXa, XIa and XIIa).
Heparin is a naturally occurring molecule that exists in the liver and in mast cells.
It acts by forming a complex with antithrombin and markedly increasing its activity in inhibiting these clotting factors.
Heparin is also able to inhibit thrombin directly.
It acts by forming a complex with antithrombin and markedly increasing its activity in inhibiting these clotting factors.
Heparin is also able to inhibit thrombin directly.
Heparin is a highly anionic mucopolysaccharide acid.
It is highly sulphated and has a wide range of molecular weights (3000 to 30,000 Daltons)
It is highly sulphated and has a wide range of molecular weights (3000 to 30,000 Daltons)
Unfractionated Heparin
This preparation of heparin involves, as the name suggests, a mixture of heparin molecules of all different sizes.
The larger heparin molecules have a greater affinity for inhibiting thrombin itself.
The larger heparin molecules have a greater affinity for inhibiting thrombin itself.
Pharmacokinetics
Due to its highly anionic nature it is highly protein bound in the plasma and is inactive if administered orally, instead being given by the intravenous or subcutaneous route (poor bioavailabilty from this last route though).
It also has poor lipid solubility and so doesn't cross the blood brain barrier or placenta.
As such it is most commonly administered via an IV infusion, but IV bolus dosing is also possible.
It also has poor lipid solubility and so doesn't cross the blood brain barrier or placenta.
As such it is most commonly administered via an IV infusion, but IV bolus dosing is also possible.
Its metabolism is via endothelial cells and the liver.
At low doses the half life is very short due to rapid metabolism (30 -60 mins) but this increases with higher doses.
At low doses the half life is very short due to rapid metabolism (30 -60 mins) but this increases with higher doses.
Adverse Effects
- Haemorrhage - Unsurprisingly the main complications arising from excessive dosage
- Osteoporosis - a possible adverse effects due to heparin interfering with mineral deposition
- Hyperkalaemia - thought to be a result of inhibition of aldosterone secretion by heparin after long duration use of heparin (risk increasing with increasing duration).
- Thrombocytopenia - Two types of thrombocytopenia can result from heparin use:
- Type 1 is a non immune based depletion of platelets that occurs within 4 days of initiation of therapy, is self limiting and doesn't require specific treatment or cessation of heparin use. It results from the direct effect of heparin on the platelets.
- Type 2 heparin induced thrombocytopenia (HIT) is a more serious complication resulting from the generation of antibodies. These complex with the heparin molecules and platelet factor 4 on the surface of platelets. There is activation of platelets through this process and subsequent thromobosis. Morbidity and mortality is high from the range of resulting thrombotic pathology (e.g. pulmonary embolism, stroke). Onset is usually between 5 an 14 days after initiation of heparin therapy.
Clinical Application
As mentioned above, unfractionated heparin is generally used therapeutically via a continuous infusion.
Different hospital trusts tend to have different infusion protocols where the rate of infusion is adjusted based on the measurement of the activated partial thromboplastin time (APTT).
The APTT is used as the clotting factors most affected by heparin/antithrombin are in the intrinsic as well as the common pathway (click here for a review of the tests of clotting).
Different hospital trusts tend to have different infusion protocols where the rate of infusion is adjusted based on the measurement of the activated partial thromboplastin time (APTT).
The APTT is used as the clotting factors most affected by heparin/antithrombin are in the intrinsic as well as the common pathway (click here for a review of the tests of clotting).
An increase of the APTT to about 1.5-2 times longer than the normal range is generally used.
Heparin can be reversed by protamine.
Heparin can be reversed by protamine.
Low Molecular Weight Heparin (LMWH)
e.g. Dalteparin, Tinzaparin, Enoxaparin
You won't be surprised to find that the LMWHs a made up the heparin molecules with a low molecular weight (between 2000 and 8000 Daltons).
They have many advantages over unfractionated heparin in clincal practice:
LMWHs have their action more through inactivation of factor Xa and little action on thrombin or the other clotting factors, as unfractionated heparin does.
They have many advantages over unfractionated heparin in clincal practice:
- More predictable anticoagulant effects, negating the need for monitoring
- Longer duration of action allowing once daily dosing
- Reduced incidence of HIT
LMWHs have their action more through inactivation of factor Xa and little action on thrombin or the other clotting factors, as unfractionated heparin does.
Pharmacokinetics
Low molecular weight heparins are comparatively well absorbed from the subcutaneous route and hence this is their general mode of administration.
I undergoes both hepatic metabolism and renal elimination.
I undergoes both hepatic metabolism and renal elimination.
Clinical Application
Dosing is generally given as once or twice daily dose based on weight.
As described above, no monitoring is required for this.
As it is factor Xa which is the greatest affected by the LMWHs, testing of factor Xa inhibition is one laboratory means of assessing their activity, but this isn't routinely done (or indeed needed) in clinical practice.
Unlike unfractionated heparin, LMWH is not fully reversed by protamine.
As described above, no monitoring is required for this.
As it is factor Xa which is the greatest affected by the LMWHs, testing of factor Xa inhibition is one laboratory means of assessing their activity, but this isn't routinely done (or indeed needed) in clinical practice.
Unlike unfractionated heparin, LMWH is not fully reversed by protamine.
Protamine
Protamine is an interesting protein that was initially derived from fish sperm.
It is highly cationic in nature, contrasting with the highly anionic heparin molecules.
This property allows in to bind with the heparin molecules and form an inactive complex that is ultimately removed from the body by the reticuloendothelial system.
As such it can be considered to be something of an antidote to heparin, though its effects on the LMWHs is not complete.
It is highly cationic in nature, contrasting with the highly anionic heparin molecules.
This property allows in to bind with the heparin molecules and form an inactive complex that is ultimately removed from the body by the reticuloendothelial system.
As such it can be considered to be something of an antidote to heparin, though its effects on the LMWHs is not complete.
Clinical Application
It is given intravenously with the dosing:
1mg = reversal of 100 units of heparin
1mg = reversal of 100 units of heparin
It can cause histamine release and potentially hypotension on administration and hence is given as a slow infusion.
Pulmonary hypertension is also a recognised adverse effect.
Pulmonary hypertension is also a recognised adverse effect.