Ventilation
Last updated 26th February 2019 - Tom Heaton
Ventilation refers to the movement of gas into and out of the lungs.
It can be considered as the first step in allowing gas exchange.
It can be considered as the first step in allowing gas exchange.
Lung Volumes
An important starting place is to think about the constituent volumes of the lungs, and create some definitions.
The total ‘volume’ of the lungs is variable depending on the person (we shall use 6L as an average), but the whole of the lungs don’t participate in every breath (i.e. the lung volume doesn’t change from 0 to 6L with each breath).
Instead, it oscillates between different ‘volumes’ in several different ways.
I am using the term volume in inverted commas here, as there is an important part of the nomenclature that will be needed:
A volume is specific defined component of the lung cycle.
A capacity is a summation of several volumes.
As we can see, when I described the total ‘volume’ of the lungs, what the technical definition is is the total lung capacity.
The total ‘volume’ of the lungs is variable depending on the person (we shall use 6L as an average), but the whole of the lungs don’t participate in every breath (i.e. the lung volume doesn’t change from 0 to 6L with each breath).
Instead, it oscillates between different ‘volumes’ in several different ways.
I am using the term volume in inverted commas here, as there is an important part of the nomenclature that will be needed:
A volume is specific defined component of the lung cycle.
A capacity is a summation of several volumes.
As we can see, when I described the total ‘volume’ of the lungs, what the technical definition is is the total lung capacity.
Let’s discover the different volumes and capacity of the lungs (we shall use some roughly usable values for example purposes - about those of an adult male).
A good way to help picture this is to imagine the volumes with someone attached to a spirometer.
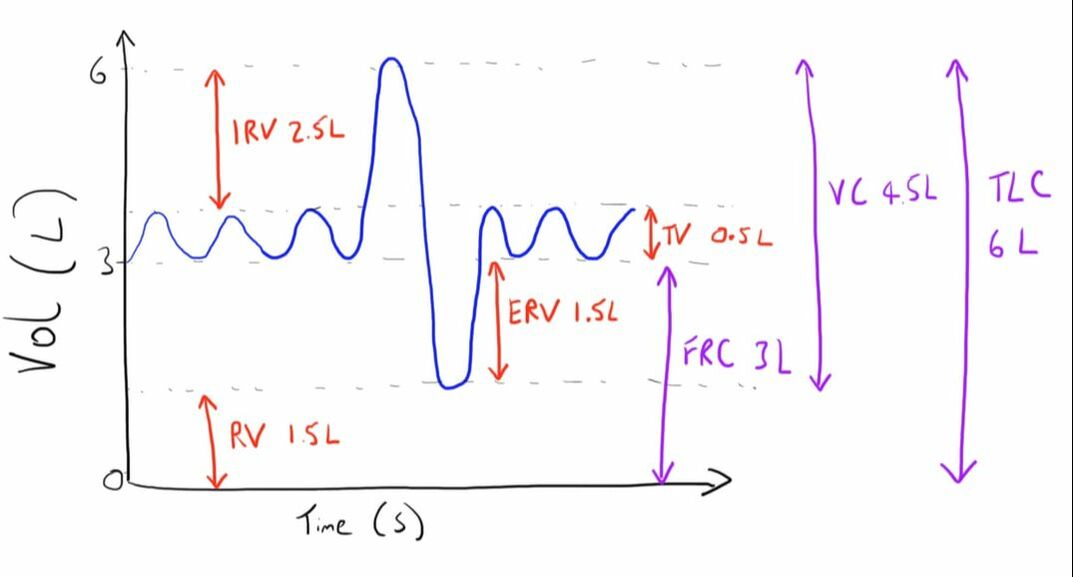
The figure below shows a graph of time (x axis) against volume (y axis).
The patient is breathing normally, and then takes a maximally deep breath in followed by a maximully deep breath out.
A good way to help picture this is to imagine the volumes with someone attached to a spirometer.
The figure below shows a graph of time (x axis) against volume (y axis).
The patient is breathing normally, and then takes a maximally deep breath in followed by a maximully deep breath out.
Imagine if we fully exhale as much as we can, as noted, we can’t get our lung volume down to zero.
This remaining ‘volume’ of air in the lungs is termed the residual volume.
This value is about 1.5L.
However, we don’t normally get to this point of maximal emptying during normal everyday breathing - we are usually breathing at a point ‘above’ this volume.
As such, the air that we must forcefully exhale to get down to this level is termed the expiratory reserve volume.
This is also usually around 1.5L
You can see that if we add this volume to our residual volume, we end up with the ‘volume’ of air that is usually in our lungs during normal everyday breathing (at the end of each out breath to be specific).
We term this the functional residual capacity, and can be estimated as 3L.
I mentioned that we breathe in and out ‘normally’ when we aren’t asked to perform special maneuvers.
We term this ‘volume’ of air that we move when doing this as the tidal volume.
This is usually around 500ml.
We can therefore see that usually we have 3L of air in our lungs, and then we breathe in and then out 500ml of air on top of this.
However, we also have the ability to breathe in an extra amount..
If we think about just after we have breathed in ‘normally’, we can then continue to breathe in as much as possible until our lungs are unable to expand any further.
This additional ‘volume’ that we have just breathed in is termed the inspiratory reserve volume.
An additional calculated ‘volume’ that hasn’t been mentioned is the vital capacity.
This is the volume of air that can be expired if you fill your lungs up maximally, and then exhale maximally.
If we think about it, this is composed of the inspiratory reserve volume, the tidal volume and the expiratory reserve volume.
This remaining ‘volume’ of air in the lungs is termed the residual volume.
This value is about 1.5L.
However, we don’t normally get to this point of maximal emptying during normal everyday breathing - we are usually breathing at a point ‘above’ this volume.
As such, the air that we must forcefully exhale to get down to this level is termed the expiratory reserve volume.
This is also usually around 1.5L
You can see that if we add this volume to our residual volume, we end up with the ‘volume’ of air that is usually in our lungs during normal everyday breathing (at the end of each out breath to be specific).
We term this the functional residual capacity, and can be estimated as 3L.
I mentioned that we breathe in and out ‘normally’ when we aren’t asked to perform special maneuvers.
We term this ‘volume’ of air that we move when doing this as the tidal volume.
This is usually around 500ml.
We can therefore see that usually we have 3L of air in our lungs, and then we breathe in and then out 500ml of air on top of this.
However, we also have the ability to breathe in an extra amount..
If we think about just after we have breathed in ‘normally’, we can then continue to breathe in as much as possible until our lungs are unable to expand any further.
This additional ‘volume’ that we have just breathed in is termed the inspiratory reserve volume.
An additional calculated ‘volume’ that hasn’t been mentioned is the vital capacity.
This is the volume of air that can be expired if you fill your lungs up maximally, and then exhale maximally.
If we think about it, this is composed of the inspiratory reserve volume, the tidal volume and the expiratory reserve volume.
Physiological Volumes
The volumes that we have discussed are taken for the respiratory system as a whole.
Whilst this may be of some use, as it is what is routinely measured, it doesn’t actually have complete physiological applicability.
This is because not all of the lungs are involved in gas exchanges, which is the key purpose of the lungs.
If we do not take this into account, such volumes may be misleading.
The term deadspace is used to refer to gas which is part of ventilation, but is not involved in gas exchange.
This can be either:
Whilst this may be of some use, as it is what is routinely measured, it doesn’t actually have complete physiological applicability.
This is because not all of the lungs are involved in gas exchanges, which is the key purpose of the lungs.
If we do not take this into account, such volumes may be misleading.
The term deadspace is used to refer to gas which is part of ventilation, but is not involved in gas exchange.
This can be either:
- Anatomical deadspace
- Physiological deadspace
Anatomical Deadspace
This is probably the easiest to understand.
As previously noted, the respiratory system has a conducting component (trachea, bronchi, etc.) whose role is to transport gas in a way that creates optimal gas exchange conditions (repeated division to produce a large surface area).
However, this conducting system is unable to play a role in gas exchange so whilst it serves a very important role in creating the conditions, is essentially wasted spaced when actually thinking about the gas exchange.
This volume is made up of all the volumes of air within the conducting system and usually equates to about 150ml in the adult.
This is fairly fixed, but may increase with vigorous inspirations where the surrounding tissue pulls open the airways further.
As previously noted, the respiratory system has a conducting component (trachea, bronchi, etc.) whose role is to transport gas in a way that creates optimal gas exchange conditions (repeated division to produce a large surface area).
However, this conducting system is unable to play a role in gas exchange so whilst it serves a very important role in creating the conditions, is essentially wasted spaced when actually thinking about the gas exchange.
This volume is made up of all the volumes of air within the conducting system and usually equates to about 150ml in the adult.
This is fairly fixed, but may increase with vigorous inspirations where the surrounding tissue pulls open the airways further.
Physiological Deadspace
This is defined as the gas volume that does not play a role in gas exchange.
As can be easily seen, this includes this anatomical deadspace, and in normal conditions the values may be very similar.
However, physiological deadspace may also include additional volumes that are not just part of the anatomical deadspace.
An example is a portion of lung which has no pulmonary blood supply.
Although the gas in entering alveolar space, without a blood-gas interface, no gas exchange can occur and so that volume is deadspace.
This is more important in disease conditions.
The points discussed allow us to calculate some other important values.
Minute Ventilation
This is the volume of air being moved each minute:
Minute ventilation = respiratory rate x tidal volume
E.g. 12 x 500ml = 6L/min
Alveolar ventilation
This is the volume of air that is actually entering the alveoli during each minute.
The volume of air entering the alveoli is simply the tidal volume minus the anatomical deadspace, which can be fairly reliably estimated:
Alveolar ventilation = respiratory rate x (tidal volume - anatomic deadspace)
E.g. 12 x (500-150) = 3.8L
Closing Volume
This is another clinically relevant value.
It is the volume of gas remaining in the lungs when the small airways start to close.
It increases with age.
At 40 years it will encroach on the FRC when in the supine position.
At 70 years it will encroach on the FRC when in the standing position.
As can be easily seen, this includes this anatomical deadspace, and in normal conditions the values may be very similar.
However, physiological deadspace may also include additional volumes that are not just part of the anatomical deadspace.
An example is a portion of lung which has no pulmonary blood supply.
Although the gas in entering alveolar space, without a blood-gas interface, no gas exchange can occur and so that volume is deadspace.
This is more important in disease conditions.
The points discussed allow us to calculate some other important values.
Minute Ventilation
This is the volume of air being moved each minute:
Minute ventilation = respiratory rate x tidal volume
E.g. 12 x 500ml = 6L/min
Alveolar ventilation
This is the volume of air that is actually entering the alveoli during each minute.
The volume of air entering the alveoli is simply the tidal volume minus the anatomical deadspace, which can be fairly reliably estimated:
Alveolar ventilation = respiratory rate x (tidal volume - anatomic deadspace)
E.g. 12 x (500-150) = 3.8L
Closing Volume
This is another clinically relevant value.
It is the volume of gas remaining in the lungs when the small airways start to close.
It increases with age.
At 40 years it will encroach on the FRC when in the supine position.
At 70 years it will encroach on the FRC when in the standing position.
Links & References
- West. B. Respiratory physiology: the essentials (9th ed). 2012
- Cross, M. Plunkett, E. Physics, pharmacology and and physiology for anaesthetists: Key concepts for the FRCA. Cambridge University Press. 2010.